Imagine a day in the future when you arrive at the hospital for your annual GI screening. You swallow a magnetic camera capsule, lie down comfortably and watch a movie while a robot named SAMM (Spherical Actuator Magnetic Manipulator) sweeps painlessly over your stomach and abdomen, gently driving the capsule forward through your GI tract to locate irregularities or potentially malignant tissue growth. No sedation, no invasive endoscope, and no recovery time required.
In his Telerobotics Lab, University of Utah mechanical engineering associate professor Jake Abbott and his team are engineering the solutions that will make this dream a reality. And they are betting that patient compliance will improve dramatically with a less-invasive method of detection. Despite the fact that colorectal cancer is the third leading cause of cancer death in the U.S., only 67% of individuals age 50 to 75 get regular colonoscopies.
Other capsule screening approaches are available but are used primarily in the small bowel and rely on the body’s natural peristalsis to move and eliminate the device. Abbott’s concept contains an internal magnet, a microprocessor and a wireless transmitter. A robotic system hovering over the body locates the magnetic capsule and drives it forward through the entire GI tract while sending real-time images to a computer screen. An important feature of Abbott’s device is an external screw thread that enables the capsule to rotate continuously but gently through the complex folds and bends of intestinal tissue.
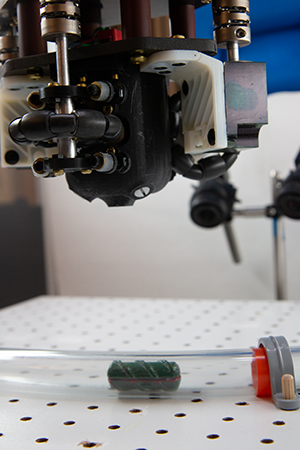 “Much of the prior research done on helical magnetic swimmers and screws has utilized electromagnetic coil arrangements for control, but these are difficult to scale up to the size of a human body. Also, electromagnetic coils generate heat, which is problematic for applications inside the human body,” Abbott explained. “We have proven that it is possible to control such a device using a single permanent magnet moved and rotated dynamically through space.”
“Much of the prior research done on helical magnetic swimmers and screws has utilized electromagnetic coil arrangements for control, but these are difficult to scale up to the size of a human body. Also, electromagnetic coils generate heat, which is problematic for applications inside the human body,” Abbott explained. “We have proven that it is possible to control such a device using a single permanent magnet moved and rotated dynamically through space.”
While the lab is currently studying the gastrointestinal tract, the technology could eventually be adapted to other places in the body. It’s one of several robotic systems in his Telerobotics Lab that focus on medical applications. Many of Abbott’s systems involve miniature robots that are controlled and moved by magnetic fields.
“Microscale and mesoscale robots have the potential to revolutionize many aspects of medicine. I believe these untethered, wirelessly controlled and powered devices will make existing therapeutic and diagnostic procedures less invasive and will enable new procedures never before possible,” said Abbott.
Abbott is also applying magnetic methods to improve the surgical insertion of cochlear implants, which are long, thin electrode arrays that stimulate nerves in the inner ear to provide hearing to a person who is deaf. In the vision of Abbott and his colleagues, a small magnet is attached to the tip of the device which is robotically inserted into the cochlea as it is magnetically guided into place.
“This is a novel, minimally invasive way to implant cochlear devices unlike anything that has ever existed,” he said. “Current implantation procedures are traumatic and often result in the clinician accidentally puncturing a critical membrane in the cochlea, resulting in a loss of any residual hearing the patient might have. Our goal is to eliminate the risk of membrane puncture and to make the entire insertion less traumatic to the delicate cochlear structures.
Abbott is definite in his assertion that the robotic systems he creates are designed to assist clinicians, not replace them. This is the goal of his research in telerobotic retinal surgery, conducted with collaborators at Moran Eye Center, with the support of Intuitive Surgical Inc., and the National Eye Institute.
Forces experienced during retinal surgery are below the limit of human sensation and the surgeon must rely on visual feedback only. This puts the retina at great risk where surgical error of a few micrometers can result in the instrument exerting damaging force, causing loss of vision. In addition, many of the up-and-coming therapeutic protocols in ophthalmology, such as subretinal injection of stem cells and gene therapies, are beyond the limits of human ability. A surgeon’s hand tremor combined with patient movement due to breathing and snoring limits the surgeon’s ability to deliver the therapy to a precise location below the retina.
 Abbott’s team has developed a robotic manipulator that is more precise than all prior systems designed for robot-assisted eye surgery. At the same time, the system is small and light enough to be mounted on the patient’s head using a helmet-like device that Abbott believes will help passively compensate for much of the error caused by patient movement due to breathing and snoring. The goal of the project is to incorporate existing disposable instruments, while delivering submicron precision at the retina. The current model of the robotic manipulator is designed to facilitate a quick change of instruments and to enable the surgeon to easily and safely pull back the instrument when needed.
Abbott’s team has developed a robotic manipulator that is more precise than all prior systems designed for robot-assisted eye surgery. At the same time, the system is small and light enough to be mounted on the patient’s head using a helmet-like device that Abbott believes will help passively compensate for much of the error caused by patient movement due to breathing and snoring. The goal of the project is to incorporate existing disposable instruments, while delivering submicron precision at the retina. The current model of the robotic manipulator is designed to facilitate a quick change of instruments and to enable the surgeon to easily and safely pull back the instrument when needed.
Abbott’s passion for medical robotics was fueled as a graduate student at the U working on human-robot systems under U mechanical engineering professor Sandy Meek. After completing his master’s degree, a move to Maryland for his wife’s graduate studies led him to pursue a doctoral degree at Johns Hopkins where he studied with Dr. Allison Okamura, now at Stanford, one of the world’s leading experts in haptics in robotics and medicine. That was followed by three years as a postdoctoral researcher at ETH Zurich in Switzerland working with Dr. Brad Nelson, a pioneer in microrobotics and the use of magnetics in robotics. Abbott joined the University of Utah in 2008 and is proud to call Utah his home.
Reprinted with permission from the University of Utah College of Engineering Fall 2019 Research Report